Oh good. They should make a hit tv show about this. Maybe base it on a game and put it on HBO?
Climate - truthful information about climate, related activism and politics.
Discussion of climate, how it is changing, activism around that, the politics, and the energy systems change we need in order to stabilize things.
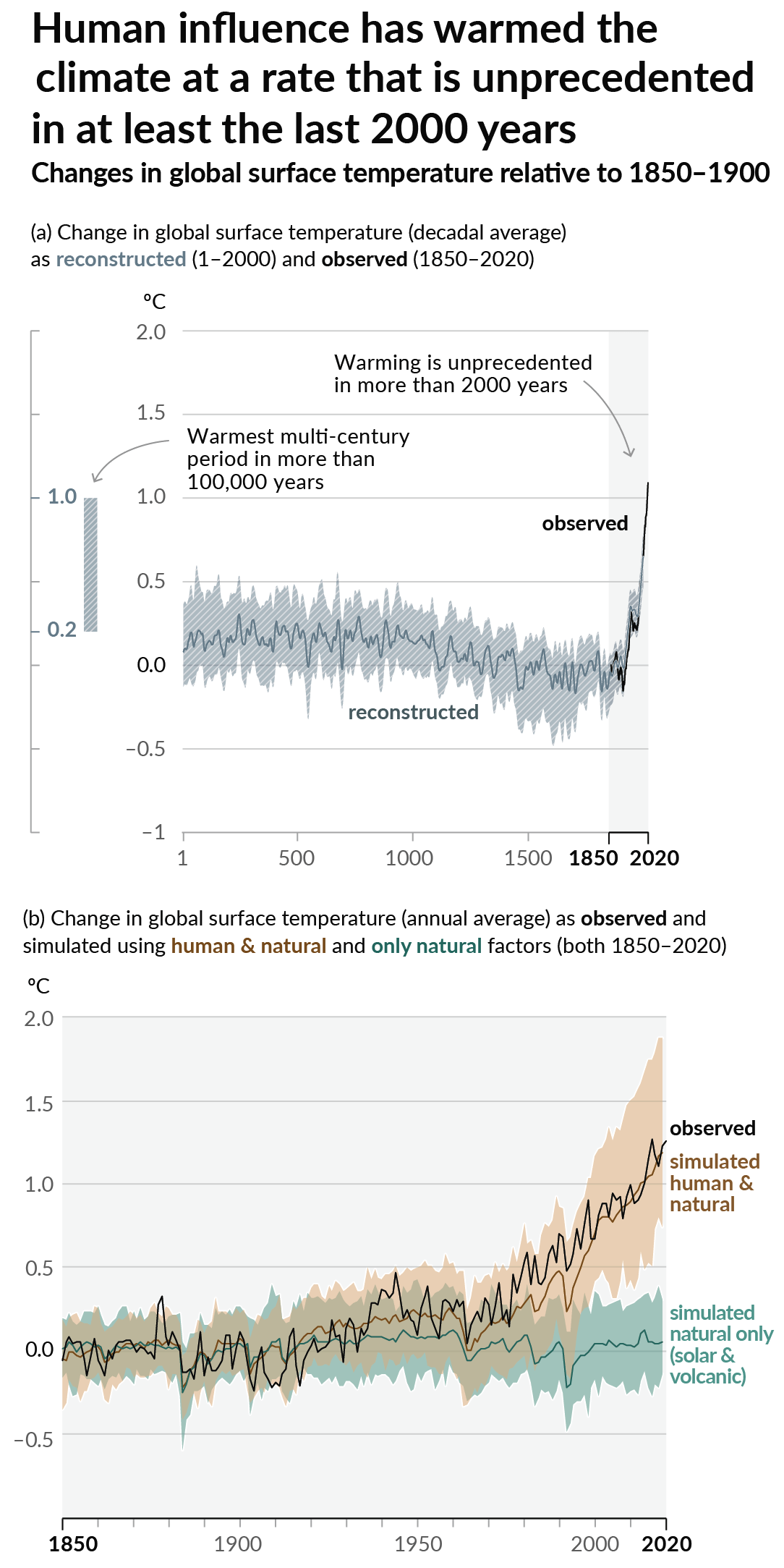
As a starting point, the burning of fossil fuels, and to a lesser extent deforestation and release of methane are responsible for the warming in recent decades:
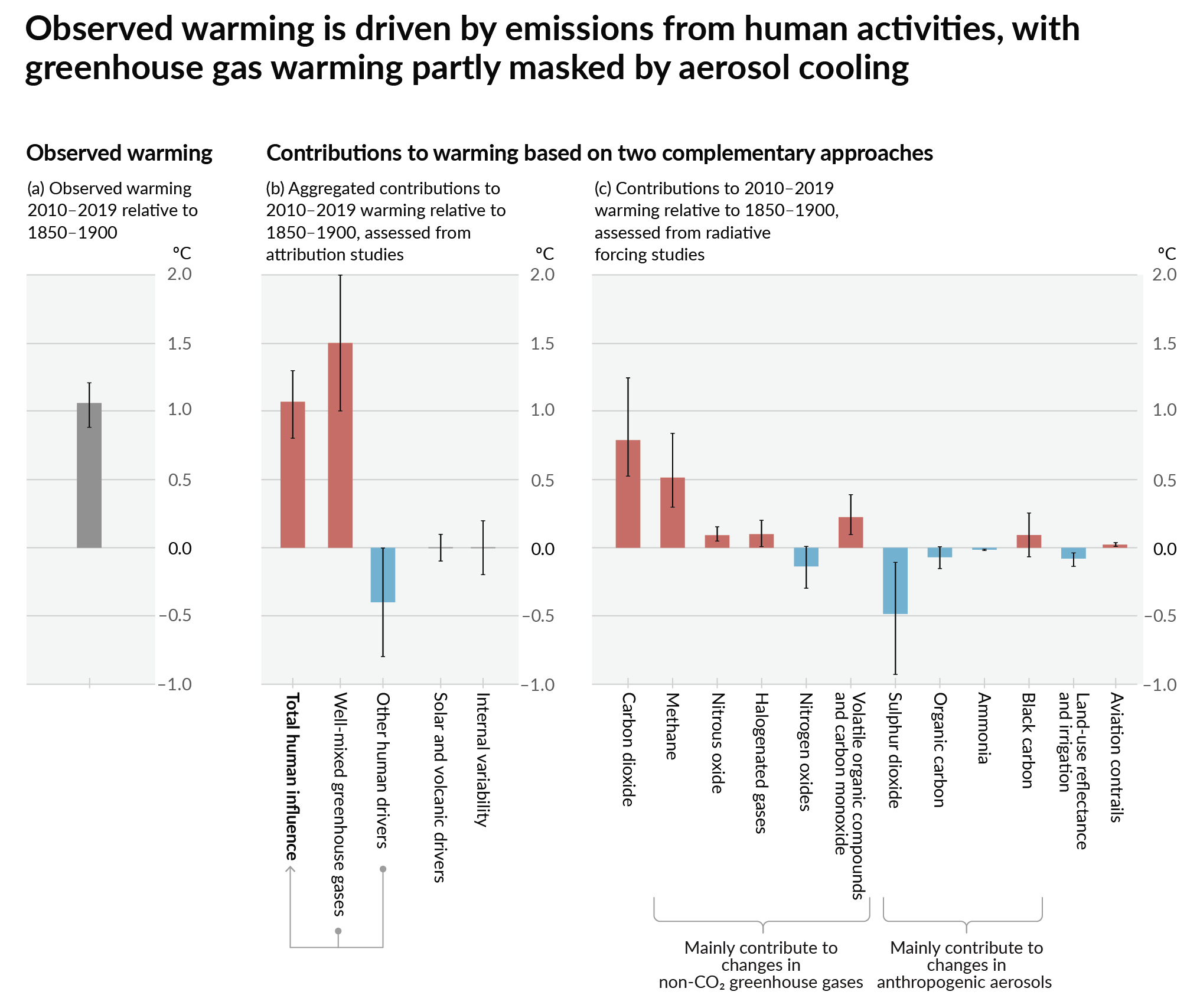
How much each change to the atmosphere has warmed the world:
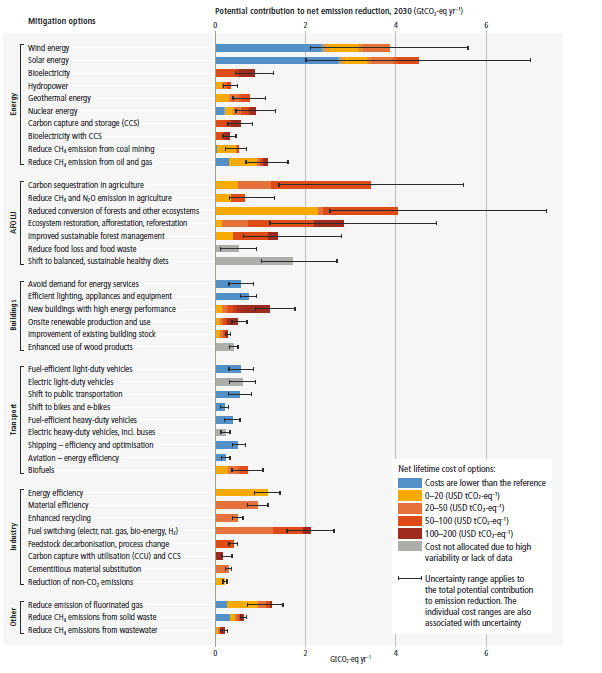
Recommended actions to cut greenhouse gas emissions in the near future:
Anti-science, inactivism, and unsupported conspiracy theories are not ok here.
Isnt it kinda weird that apnews found that important enough to mention? Like hey a global crisis is about to cause another global crisis, no idea what to do about it, but HBO has a cool TV show about it!
Btw not meaning to criticize your comment, you're doing what social media is intended for, just thought it weird in the article.
Interestingly enough, the game was called Sid Meier's Alpha Centauri.
Only if it includes lots of dad jokes.
Interesting speculation but wish there was a bit more information in the article. For anyone interested, this particular species of candida is considered highly dangerous because it is resistant to most of the antifungal medications we currently use
but thats stated
>“It’s a potentially multi-drug resistant pathogen with the ability to spread very efficiently in healthcare settings,” he said. “We’ve never had a pathogen like this in the fungal infection area.” It is nearly always resistant to the most common class of antifungal medication, and is sometimes also resistant to another medication primarily used for severe catheter fungal infections in hospitals.
Apologies, I meant that I wanted to know how they came to the conclusion that climate could be affecting the prevalence. I'm not denying their claim, just curious what evidence they have.
I may have missed your quoted section because I opened the link on mobile and couldn't stand how disruptive the page was without ad block.
A shit you made me read it again too and they also say that
“I think the way to think about how global warming is putting selection pressure on microbes is to think about how many more really hot days we are experiencing,” said Casadevall of Johns Hopkins. “Each day at (100 degrees Fahrenheit, or 37.7 degrees Celsius) provides a selection event for all microbes affected — and the more days when high temperatures are experienced, the greater probability that some will adapt and survive.”
Idk, not a scientist. Seems like one of those complex chain reaction things, not a question of direct evidence for a single causing factor. Most of that stuff prefers warm temperatures and humid environments. Water from floods for example is full of delicious food for all kinds of organisms that can harm us. Also possible that the warming and seasonal weather extremes will speed up their evolution and make them generally stronger. Then combine that with the growing antibiotic resistance, and even weak and lame stuff like legionella will very soon be a greater danger.
Oh good... Another fun twist in this great timeline
Well good thing I've played through both TLoU games. And I watched the series. I know exactly what to do.
Not eat wheat.
Did they explain how it survived the cooking process?
I mean flour makes a cloud whenever you open the packaging. It’s equally possible that the spores were inhaled before cooking.
Very small heat shields.
John Hannah warned us about this in 1968.
The Wikipedia article is perhaps more helpful than the news story.
Fungi are much closer to animals in evolutionary terms than bacteria. Many substances which effectively kill fungi are harmful to animals, including humans. Antibacterial antibiotics are mostly useless. There exist antifungal antibiotics, but their selection is limited. Vaccination is possible, but not yet feasible in people. A mouse has been successfully vaccinated against Candida auris and gained some protection.
Fungal diseases are generally slower compared to viral (very fast) and bacterial (fast) diseases, but harder to wipe out.
This fungus is generally a threat in hospitals, where people with compromised immune systems and open wounds may be encountered. A description of a Candida outbreak in a medical setting can be found here. It broke out in the intensive care unit of a London hospital. Many patients had wounds, catheters or intravenous lines. They resorted to isolating every patient, disinfecting rooms with agressive substances, using plentiful chrorhexidine to prevent infection via wounds and lines, and antifungals to treat patients.
Nobody died at the Royal Brompton Hospital, but the mess was severe. Candidasis of the blood (typically after entry through a wound) has a high level of mortality. Whether it is a case fatality ratio or infection fatality ratio - no idea. With new diseases, one typically learns the CFR first and IFR much later, except in hospitals where you can test every person.
Next year, the US CDC described it as a "catastrophic threat". Antifungals that target Candida with less side effects, and a vaccine against it, are highly sought after. I trust they will be found, but not soon - this is not COVID, it spreads slowly, so everyone isn't running (yet) to put a lid on it.
The hypothesis about how it crossed to humans, is summarized by this picture. Wetlands -> thermotolerance -> birds -> agricultural setting -> humans -> hospital setting. I'm not sure if this guess is correct, but it has explanatory value.
Apparently it was capable of crossing species barriers anyway, because it's a generic sort of decomposer fungus - it needs nothing highly specific, and breaks down a variety of biomolecules for food. What is notable: it gained resistance to antifungals before entering people. Probably through agricultural use.
I, for one, welcome our new mushroom overlords
This isn't a twist, it's just the forecast. Mycologists have been warning about this for a while
"Its mortality rate has been estimated at 30% to 60%, and it’s a particular risk in healthcare settings for people already with serious medical problems."
Well least not 100% and controlling brain... yet
That's the rate when an infection establishes itself in blood. In a known outbreak (Royal Brompton Hospital), I recall that 9 patients out of 50 (18%) developed candidemia, but none of them died.
However, a study from India reports:
Among 1,400 ICU-acquired candidemia cases (overall incidence of 6.51 cases/1,000 ICU admission), 65.2 % were adult. Though the study confirmed the already known risk factors for candidemia, the acquisition occurred early after admission to ICU (median 8 days; interquartile range 4-15 days), even infecting patients with lower APACHE II score at admission (median 17.0; mean ± SD 17.2 ± 5.9; interquartile range 14-20). The important finding of the study was the vast spectrum of agents (31 Candida species) causing candidemia and a high rate of isolation of Candida tropicalis (41.6 %). Azole and multidrug resistance were seen in 11.8 and 1.9 % of isolates. Public sector hospitals reported a significantly higher presence of the relatively resistant C. auris (8.2 vs. 3.9 %; p = 0.008) and C. rugosa (5.6 vs. 1.5 %; p = 0.001). The 30-day crude and attributable mortality rates of candidemia patients were 44.7 and 19.6 %, respectively. Logistic regression analysis revealed significant independent predictors of mortality including admission to public sector hospital, APACHE II score at admission, underlying renal failure, central venous catheterization and steroid therapy.
Notes:
-
C. auris is observed together with other pathogens like C. rugosa and C. tropicalis, leading to the question of which of them is the killer, or whether co-infection is the killer
-
the mortality rate is given as a percent of people who developed candidemia (had Candida infections in their bloodstream), not as a percent of the total; upon hasty reading this can fool a person, and has fooled people before
-
the mortality rate is split into two variables: crude mortality (the patient is dead, the patient tests positive) and attributable mortality (the patient is dead, we can see how Candida killed the patient)
-
they found correlations which increased the risk; since they list "admission to a public sector hospital" among the factors, low standards of care in the Indian public healthcare system, or lack of experience in dealing with Candida (including wrong treatment protocols) may explain part of excess mortality
The study from Venezuela (a country afflicted with civil conflict and poverty) reports:
A total of 13 critically ill pediatric and 5 adult patients, with a median age of 26 days, were included. All were previously exposed to antibiotics and multiple invasive medical procedures. Clinical management included prompt catheter removal and antifungal therapy. Thirteen patients (72%) survived up to 30 days after onset of candidemia. AFLP fingerprinting of all C. auris isolates suggested a clonal outbreak. The isolates were considered resistant to azoles, but susceptible to anidulafungin and 50% of isolates exhibited amphotericin B MIC values of >1 μg/ml.
Unfortunately, the summary does not give adequate clues to understand the underlying conditions of the people (as I notice - mostly children). It mentions they were "critically ill", but doesn't mention if they were critically ill with Candida or before getting Candida. With such statistics as given in the summary - it is truly hard to evaluate the danger posed by a pathogen, because it's hard to isolate it from other factors. However, 30-day mortality was 28%, which is miserable.
My main conclusion seems to be: the first line of defense is having a hospital system that is ready to detect and deal with Candida. If this exists, many deaths can be avoided.
Of course, vaccination would be far preferable to combating it at a later stage.
shitake
big fungus